Manifested as excessive and consistently recurrent emotional distress on account of past psychological traumas. The distress did not present with daytime flashbacks or nightmares, feelings or symptoms of significant anxiety, nor panic. It is interesting to note that despite management with medications for anti-depression treatment, the patient remained cyclically refractive, regarding her affective mood. On two occasions, when the patient initially agreed on a discharge date, on the morning of discharge, she stated, "I'm not ready. Cognitive behavioral therapy and supportive psychotherapy services were referred to follow up as an outpatient telehealth treatment plan for the patient's mental illness. People tend to seek interaction, connections, attachments, and relationships with other people.
In fact, mental health is partly defined with regard to the strong emotional attachments to, and flexible interdependence on, close relationships we maintain with one another. But when interdependence becomes unbalanced to the degree that it is one-sided, it can become problematic, particularly if dependent personality disorder is involved. DPD can have a major impact on the ability to function in daily life.
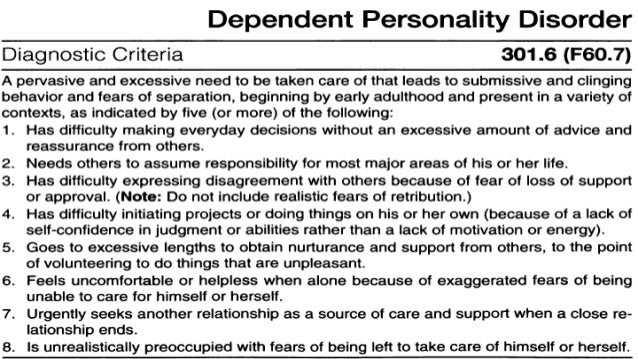
For instance, society holds expectations regarding individual decisiveness, independence, and self-reliance that are dependent on age and situation, such as physical or medical issues. A person who does not meet those expectations could face difficulty functioning in school, work, and other interpersonal situations. The Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5), provides a comprehensive framework for symptoms and classification of behavioral health conditions. However, efforts to make codependency a recognized disorder have been unsuccessful. The latest iteration of diagnostic criteria, the DSM-5, only includes dependent personality disorder as an official diagnosis, not codependency.
Dependent Personality Disorder will typically have major impacts on most areas of functioning. As an adult, there are societal expectations for independence, decisiveness, confidence, and self reliance, particularly in American culture. An individual who does not meet these expectations will have difficulty functioning in occupational, academic, and interpersonal settings. Individuals with Dependent Personality Disorder may continue to reside with their parents past their twenties, may not learn how to drive a car, may be unemployed, and not continue or complete their education.
It is noted in the DSM -5 that Individuals with Dependent Personality disorder will tolerate situations from which others would promptly withdraw, including verbal, physical and sexual abuse. Women with Dependent Personality Disorder were found to be at risk for spousal abuse. Due to economic and emotional dependence of their abusive husbands (Loas, Cormier, & Perez-Diaz, 2011). Individuals with dependent personality disorder may be viewed with pity, disgust, anger, frustration, or contempt by others, and will try the patience of others, , including their clinicians. There may be a reciprocal causality for the abuse of persons with Dependent Personality Disorder.
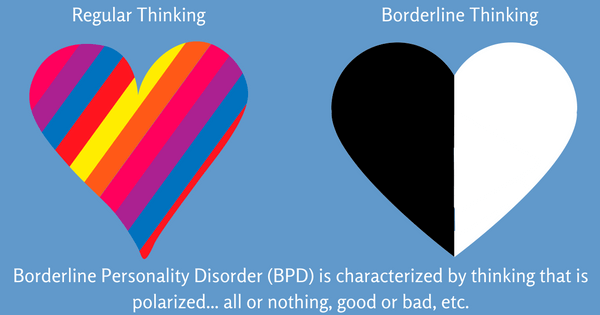
They tend to be naïve, have poor boundaries, and enter new relationships without forethought of potential risks and may be prone to exploitation by predatory individuals. In this way, a very unhealthy relationship dynamic will be established. Comorbid dependent personality disorder and borderline personality disorder is a difficult diagnosis. Both personality disorders cause troubled relationships, overly-emotional reactions, and unhealthy behaviors. The symptoms can lead to significant dysfunction in all areas of life but especially in relating to other people.
Passive Dependent Personality Disorder Symptoms Used as treatment for people with dependent personality disorder. Cognitive-behavioral therapy focuses on patterns of maladaptive thinking and seeks to eliminate them. Often people in cognitive-behavioral therapy set goals that they eventually try to achieve without relying on others.
Often the patient is receptive to the treatment and seeks help with their personal relationships. With this particular kind of therapy, the therapist will help the patient understand how they interact with others and how this contributes to their dependency issues. This particular therapies purpose is to show the patient that their dependency comes with a high price and that they do have alternatives. Another type of therapy used to treat dependent personality disorder is group therapy.
Often people taking part in group therapy must be highly motivated to see improvement. Studies show that time-limited assertiveness-training groups with very clear goals are successful. It has also been said that family or martial therapy can improve a person's independence by working on the families relationship as a whole. The goal of therapy is to help the person with DPD become more active and independent, and to learn to form healthyrelationships.
Short-term therapy with specific goals is preferred when the focus is on managing behaviors that interfere with functioning. Interpersonal therapy focuses on how mental health issues can affect relationships. After an initial assessment in the early sessions, together with a therapist the interpersonal issues will be identified and ranked in order of importance. Then the aim will be to develop a set of adjustments, and how to implement them in daily life. This type of therapy is best suited to people that have been diagnosed with dependent personality disorder, as the therapy is very targeted and usually lasts between 12 and 16 sessions.
The staff at our mental health treatment center understand how difficult these symptoms, both struggling with them and overcoming them, can be. To aid lasting recovery, Solara provides an inpatient program to clients with dependent personality disorder, giving them a place away from both dependent relationships and damaging thought and behavior patterns. Away from these things, clients can break destructive habits and learn new, healthy ones that will allow them to practice making independent decisions and build their self-confidence.
The etiology for DPD is supported by the notion that family upbringing, social-observed learning, and childhood trauma have been implicated as a causative role in dependent personality disorder. The case study patient's history aligns with childhood trauma as a causative role outlined in reported literature . It makes logical sense that children who were separated from their caregivers in some way may become adults with developed attachment or detachment issues connected to mental illness.
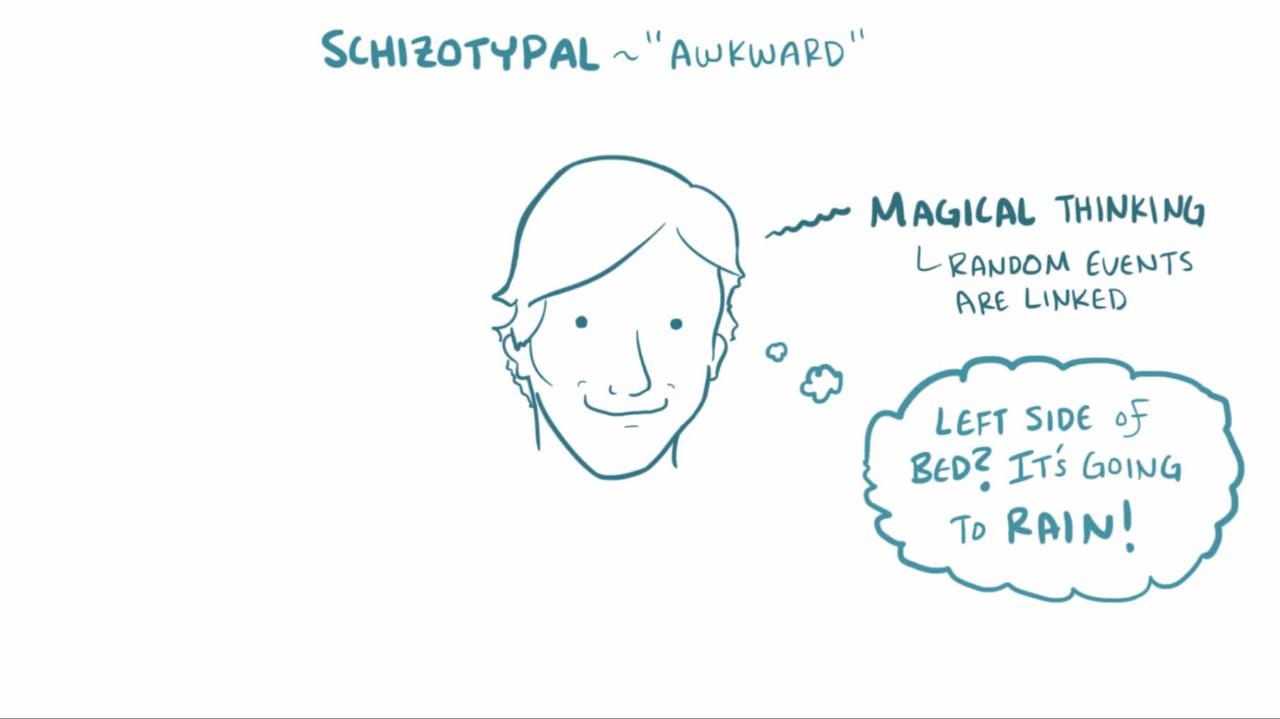
A child or an adult's negative attributes are evidenced by viewing one's self as dysfunctional or inadequate and acquiring insecure attachment relationships with others . DPD is a personality disorder characterized by a pervasive and excessive need to be taken care of. Other disorders included in Cluster C are avoidant and obsessive-compulsive personality disorders; all three show high levels of anxiety.
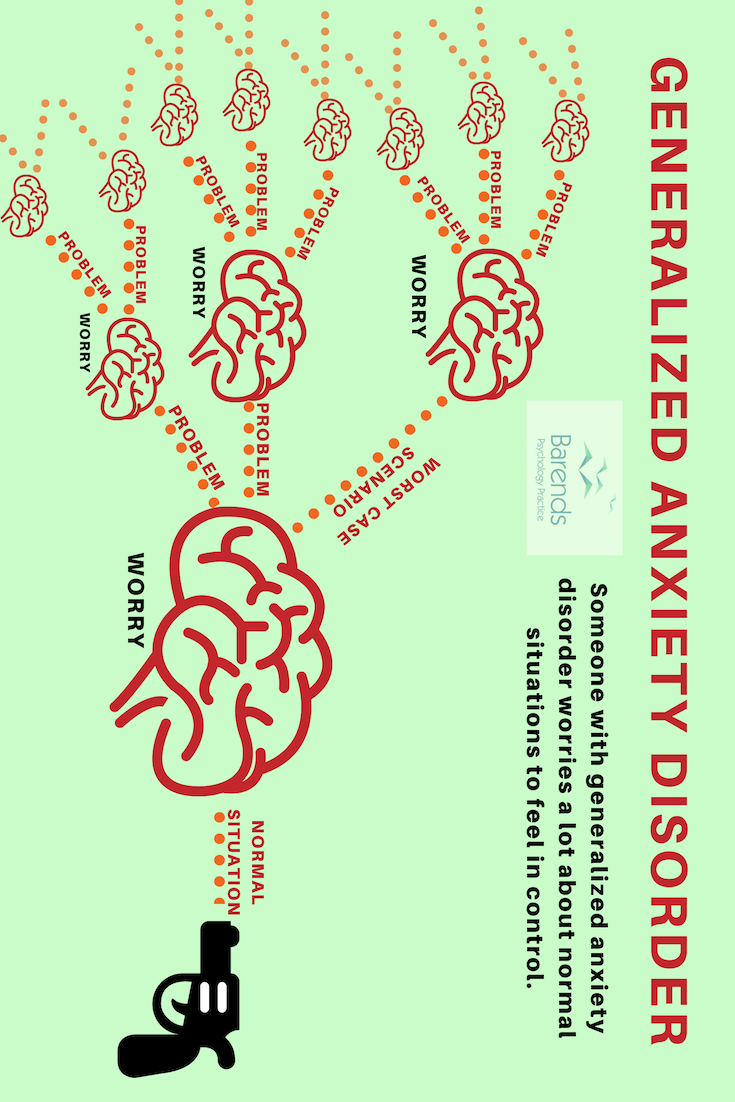
Common symptoms of dependent personality disorder include things like extreme sensitivity to criticism, fear of abandonment or separation, and a sense of helplessness when a relationship ends. Everyone experiences some level of discomfort at the end of a relationship. For example, you might feel unable to make everyday decisions, and you may need constant support or approval from others. Narcissistic Personality Disorder is an extreme version of narcissism. Moreover, it is one of the more difficult personality disorders to diagnose, because the symptomology can be mistaken for other mental health conditions or simply difficult personality traits.
Narcissistic tendencies include having grandiose ideas about oneself and one's achievements. Therefore, narcissists seek excessive admiration from other people and society as a whole. Furthermore, they become fixated on external success and control. Personality disorders are a specific type of behavioral health disorder that affect an individual's ability to function and maintain a high quality of life. People who struggle with a personality disorder may have difficulty maintaining healthy relationships and often have a skewed perception of themselves and others.
Codependent personality disorder can affect a person's quality of life and relationships, and it may occur with other mental health disorders. Certain types of psychotherapy are effective for treating personality disorders. During psychotherapy, an individual can gain insight and knowledge about the disorder and what is contributing to symptoms, and can talk about thoughts, feelings and behaviors. Psychotherapy can help a person understand the effects of their behavior on others and learn to manage or cope with symptoms and to reduce behaviors causing problems with functioning and relationships.
The type of treatment will depend on the specific personality disorder, how severe it is, and the individual's circumstances. Usually, dependent personality disorder is treated with a combination of talk therapy and medication, if necessary. Therapy focuses on adjusting negative disruptive behaviors and patterns of thinking. The goal is to increase independence through improving the ability to make everyday decisions, and to initiate and develop healthy satisfying relationships.
Treatment for DPD can be effective and improve function in daily life. Compared to other mental illnesses, dependent personality disorder isn't very common. It is only diagnosed in 0.5 to 0.6 percent of the general population. However, signs of this personality disorder can appear in virtually anyone. You may experience some symptoms of DPD throughout your life, even if you don't have this mental health condition. Schizoid personality disorder causes individuals to feel as though other people will only cause them problems, and that close relationships with others will get in the way of their day-to-day life.
These beliefs therefore mean that you tend to be uninterested in forming and maintaining relationships, even with close family members, and have no desire to be intimate with others or form emotional connections. This, in turn, can mean that people with schizoid personality disorder are aloof, detached and isolated, and find it difficult to experience pleasure and enjoyment from their everyday life. Dependent personality disorder frequently occurs in tandem with other personality-based mental illness, such as borderline, histrionic, and avoidant personality disorders . It is also believed that those diagnosed with dependent personality disorder are at an increased risk of mood and anxiety disorders.
One of the most common personality disorders, dependent personality disorder usually manifests itself in early adulthood. The disorder heavily impacts the formation and maintenance of interpersonal relationships. Those with DPD have extremely low self-esteem, an intense fear of being abandoned and noticeable helplessness.
For some with DPD, this dependence is so deeply ingrained that they may enter into—and remain in—damaging or abusive relationships because the fear of confrontation or abandonment runs so deep. To date, the altruistic type of dependent personality disorder has not been previously found on literature search engines as a topic extensively reviewed. It is recommended that more studies are done on personality disorders to utilize them as identifiable markers or primary diagnosis indicators of mental illness. A skilled clinician's capacity to efficiently conduct a psychiatry interview with personality disorders in mind may increase the likelihood of achieving a prompt clinical diagnosis.
Further advancement of dependent personality disorder subtypes and associative conditions such as adjustment disorder can spark a renaissance toward the advancement of clinical psychiatry. It is not surprising that cognitive behavioral therapy is a treatment method for DPD of various subtypes. Cognitive therapy enables a patient diagnosed with a personality disorder to understand his/her history, including childhood traumas. The self-sufficient capacity to fill themselves up, without a need to depend on others or have feelings of emptiness resolved by helping others, indicates successful treatment . Dependent personality disorder is characterized by a pervasive and excessive need to be taken care of, leading to a dependence on others to meet one's emotional and physical needs. Individuals with DPD tend to display needy or clingy behavior and have a fear of separation.
DPD also leads to difficulties in decision-making; sometimes, individuals with DPD struggle making choices as seemingly simple as 'what to wear today' without the advice and reassurance of others. The TARA for Borderline Personality Disorder's mission is to foster education and research in the field of personality disorders, like borderline personality disorder. Dependent personality disorder is a mental health issue where sufferers exhibit an excessive need to be taken care of, resulting in needy and submissive behaviour. It is categorised as a Cluster C personality disorder, which also houses avoidant personality disorder and obsessive compulsive disorder.
Cluster C personality disorders all exhibit heightened levels of anxiety; in the case of someone with dependent personality disorder, feeling alone and being helpless are the main sources. In addition, a codependent often feels compelled to take care of others and feels a need to be liked by everyone. Intimacy issues, fear of abandonment, and confusing love with pity are common traits. As a whole, these symptoms pertain to a single person or family as opposed to dependent personality disorder where the symptoms apply to people within the social network as a whole.
Taking a codependency quiz can help to better understand the symptoms and traits inherent in people who struggle with the condition. The argument against having a distinct diagnosis for codependency stems from the idea that the condition shares too much overlap with other mental health conditions to merit its own diagnosis. For example, codependency symptoms overlap significantly with dependent personality disorder , as well as borderline personality disorder . We publish material that is researched, cited, edited and reviewed by licensed medical professionals. The information we provide is not intended to be a substitute for professional medical advice, diagnosis or treatment. It should not be used in place of the advice of your physician or other qualified healthcare provider.
Dependent personality disorder can create sorrow for both those who have the illness as well as their loved ones. Signs and symptoms of dependent personality disorder may include an enduring need to be taken care of and fear of being separated from important individuals in their life. This dependent personality often displays submissive characteristics, which provokes care-giving and protective behaviors in other people. The dependent behavior may seem needy to family, friends and acquaintances. The DSM-5 defines dependent personality disorder as an excessive and pervasive need to be taken care of with behavior that is submissive, clinging and needy due to fear of abandonment.
Continue reading to learn more about this mental health condition. While dependent personality disorder can be an overwhelming and disruptive condition, it is also a treatable one. Often, a residential treatment program offers the best environment to engage in these therapies due to the intensity of care made possible by the residential milieu. As a result, they can move toward greater confidence, assertiveness, and independence.
However, when left untreated, DPD can develop into other medical and mental health conditions including depression, anxiety, avoidant personality disorder, and substance abuse. A personality disorder is a type of mental health disorder that usually begins during adolescence. Therefore, a teenage personality disorder can significantly disrupt the development of a teen's identity, relationships, and emotion regulation. Moreover, untreated personality disorders can lead to social isolation and/or substance abuse.
People who have a diagnosis of personality disorder have a tendency to develop other mental health conditions, particularly if stressed. These include psychotic illnesses, depression and drug and alcohol abuse. Developed a coping mechanism that caused her to be dependent on the desire to care for others in order to boost her self-worth or mood, and her desire to continue living. Both dependent personality disorder and BPD are characterized by fear of abandonment. In dependent personality, the individual also urgently seeks a replacement relationship to provide caregiving and support.
BPD can further be distinguished from dependent personality disorder by a chronic pattern of intense and unstable relationships. NIDA also shares that 43 percent of people in addiction treatment for non-medical use of prescription painkillers have symptoms of or are diagnosed with a mental health disorder, including anxiety and depression. These two mental health conditions are common with people with DPD. It is essential to not self-medicate with prescription opioids, alcohol, or other drugs, like marijuana. Dependent personality disorder can deeply disrupt a person's ability to function in a healthy way. As a result, the disorder often creates overwhelming distress for everyone involved.